Leishmaniasis
PKGhatak, MD
Leishmania is a flagellated protozoan of the genus Leishmania. Of the several species of Leishmania, about 20 species are infectious to humans. The flagellated tiny protozoa enter human victims from the regurgitated gut contents of female sandfly bites when the fly probes for a blood meal. There are about as many varieties of sandflies as there are leishmania species. The infectious form of the parasite is called Promastigotes. Promastigotes bind to the receptors on the skin macrophages. The parasites drop their individual flagella and enter the macrophage and continue to live inside the macrophage and at this stage, the parasite is called Amastigotes and the amastigotes multiply and infect more macrophages; eventually, macrophages of the skin, reticulo-endothelial tissue and viscera are loaded with parasites.
The human body is unable to mount an immune defense against leishmania because the parasite successfully thwarts both innate and acquired, cellular and humoral arms of the immune system. Thymic 1 cells (TH1) secrete IL-12 which transforms native T-cells into TH1 cells. TH1 cells produce TNF gamma (tissue necrosis factor gamma) and NK cells (natural killer cells). These are the resistive forces to the body. The parasite switches T-cells to TH2 cells which secrete IL-4 and IL-10 and which protect parasites from being killed.
Leishmaniasis is prevalent around the tropical and subtropical regions. The countries are separated into the Old World and the New World countries. The old world belongs to Central Asia, the Eastern shore of the Mediterranean, the Indian subcontinent, South Eastern Asia, and Eastern African countries. The new world comprises Central American and South American countries. It is estimated that between 1 and 2 million people are newly infected every year, but only a small fraction of them will develop the disease and 20,000–30,000 die each year.
An increased number of leishmania cases are seen in the last 25 years. This increase is due to globalization and climate change, air travel, sharing contaminated needles between IV drug users, being unable to detect contaminated donated blood, close human interactions with domesticated animals, particularly dogs, which serve as an intermediate host, HIV infection and blood and organ donations.
Clinical feature.
Several factors determine the nature of Leishmania clinical presentation. Besides the leishmania species and sandfly subtype, other factors are climate and the immune status of the individual. The cutaneous, mucocutaneous and visceral forms of leishmania are the main clinical types. Visceral Leishmania is better known as Kala-azar, an Indian word for Black fever. In certain endemic areas, Kala-azar is followed by dermal lesions which outwardly resemble Lepromatous leprosy and are known as post-kala-azar dermal leishmaniasis (PKDL). In Brazil mucocutaneous leishmania is known as Espundia. In the old world, the cutaneous lesions are known as Oriental Sores.
Cutaneous lesions (Oriental Sores).
The incubation period is weeks to months following the fly bite. The skin lesion may be single or multiple, dry or wet. In the new world, a single lesion is usual, multiple lesions are more common in the old world. The lesions may spread by lymphatics and satellite lesions are seen. Initially, a red papule appears and slowly but gradually progresses to a macule and ulcer. In central Asia, Afghanistan and western Pakistan, cutaneous leishmania is the common presentation.
Mucocutaneous.
Mucocutaneous presentation is mostly seen in Mexico and Brazil. Lesions on the face are associated with ulcerated lesions in the nose, mouth, pharynx and trachea. Ulcers and scar tissues produce deformities and organ dysfunction. The incubation period is 1 to 3 months. Urgent medical treatment is necessary.
Visceral.
At an earlier time, the undivided province of Bengal, India was the epicenter of kala-azar. The incidence has fallen sharply but sporadic cases are seen in Bihar, Nepal, Bangladesh, West Bengal, and the Eastern shore countries of North Africa. The incubation period is 3 to 6 months and may be as long as a year. Fever, weakness, enlarged spleen and liver are followed by a characteristic double spike of fever every day, anemia and pancytopenia, increased skin pigmentation and dryness of the skin. Dependent edema, ascites and secondary infection follow and deaths in 2 years if no treatment is available.
PKLD (post kala-azar dermal leishmaniasis).
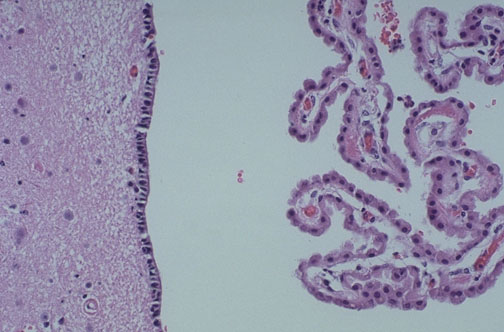
Years after visceral leishmania is treated and cured, nodular lesions appear on the face, the trunk and the limbs. The lesions are numerous and have the appearance of leprosy, except for the perception of touch and pain remains. And no spontaneous amputation of digits and toes occurs in leishmania as it happens in leprosy.
Viscerotropic leishmania.
This is a subvariety of visceral leishmania but after initial symptoms, the disease does not progress.
Diagnosis.
The parasite must be demonstrated in the samples taken from a skin biopsy and from the bone marrow biopsy in visceral leishmania.
Treatment.
CDC designated drugs used in the treatment of leishmania as orphan drugs. Anyone can contact CDC for guidance and will be assured of a supply of medications.
In 1920, Dr. Upendranath Bramhachari, a native of Kolkata, India, discovered that when Urea Stibamine was given IV it was very effective in bringing an end to the human misery in Bengal. Initially, the cure rate was 90 % and not many side effects were noted. But in the long run, safer Antimony compounds were introduced. Even today, the medical community of India pays tribute to Dr. Bramhachari for his service to humanity.
Antimonial. The pentavalent antimony (Sb V) enters macrophages and fuses with the membrane of the Lysosome of macrophages. There it is converted to Sb III (trivalent) compound. Sb III is a poison to the amastigotes.
Miltefosine. It is an oral anti-leishmania drug. It blocks the lipid metabolism of the parasite. It is also useful in children but has the potential for malignancy. Combining it with Amphotericin B and Paromomycin increases efficiency and lessens side effects.
Dr. Bramhachari.
***************************************************************************