Abnormal Red Blood Cell Morphology and its Significance
PKGhatak, MD
Blood is known as the vital fluid and that characteristic belongs to the Red Blood Cells (RBCs). The hemoglobin, contained in the RBC, avidly combines with Carbon dioxide, a waste and toxic product of cell metabolic activities; and the RBC exchanges it for Oxygen in the lungs and carries oxygen to every living cell of the body (except the cornea).
RBC is routinely tested for - size, shape, color, volume, uniformity of distribution and for any structural anomalies; and all these are reported when a CBC (complete blood count) is ordered.
No other cell in the body has been studied that thoroughly.
A normal red cell (RBC) is a disc shaped and biconcave cell without a nucleus and inclusion bodies. The red color of the cell is due to the presence of oxyhemoglobin. RBCs appear brilliant ruby color when allowed to settle in a test tube filled with normal saline.
RBCs are 7 to 8 cu mm. in diameter, the central 1/3 is paler than the periphery. Normal RBC volume (MCV) is 80 -95 fL, and the normal number of RBCs is about 5 million per cu mm. The RBC shape is fairly inform - the RWD (red cell width distribution) is 11 to 15 %.
RBCs are formed in the bone marrow from the stem cells of the Myeloid line; Erythropoietin, a hormone produced in kidneys, stimulates RBC production. In circulation, RBCs survive for 100 – 120 days. Every part of the RBC is recycled by the spleen and other scavenger cells.
Size: Abnormal size is called Anisocytosis.
Normal size RBC is called Normocyte, Microcyte is < 7 cu mm (MCV<80 fL) and Macrocyte is over 8 cu mm (MCV >95).
When Anemia is detected, the finding is reported as either normocytic, microcytic or macrocytic anemia. Normocytic anemia is seen after a recent blood loss, like an accident, fracture of long bones, or surgery. Microcytic anemia is due to iron deficiency, thalassemia, chronic inflammation, slow GI blood loss due to cancers or bleeding duodenal/gastric ulcers and sideroblastic anemia. Macrocytic anemia is seen in Pernicious anemia, Folate and Vitamin B12 deficiencies, Steatorrhea, Myelodysplastic syndrome, Liver cirrhosis, Alcoholism and Drug- use of Hydroxyurea.
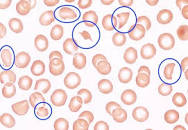
Shape: Abnormal shape is called Poikilocytosis. The abnormal shape could be Spiculated or Non-Spiculated.
Spiculated RBCs are called Burr cells, broken RBCs are known as Schistocytes resemble Napoleon hat), Helmet cells, Acanthotic cells and Dacrocytes (tear drop shaped) cells.
Non-spiculated RBC are Target cells, Ovalocytes and Stomatocytes, Pencil cells, Bite cells, Tear Drop deformities, Spherocytes and Elliptocytes.
Burr cells are seen in renal failure.
Ovalocytes and Elliptocytes are due to Hereditary causes; in addition, spherocytes are also seen in severe burns, ABO incomparable blood transfusion and acquired idiopathic hemolytic anemia.
Target cells are common in sickle cell hemoglobinopathies, thalassemia and iron deficiency anemia.
Bite cells are seen in Chronic Obstructive Pulmonary Diseases (COPD).
Stomatocytes (fish mouth like) are common in Liver disease, alcoholism, Rh-null disease and COPD.
Teardrop deformity cells are present in Myelofibrosis and pernicious anemia.
Helmet cells, Broken cells or Schistocytes in the peripheral blood are ominous signs. These cells in the blood indicate active hemolysis. Usually one of the following conditions is responsible – Decimated intravascular coagulation, TTP (thrombotic thrombocytopenic Purpura)and Thrombotic macroangiopathic anemia.
Color:
The red color of RBCs is proportional to oxyhemoglobin concentration in the cells. Based on the hemoglobin concentration per red cell, the cells are called Monochromic, Hypochromic or Hyperchromic. When color is not uniform, it is called Anisochromatic and when more than one color is present, it is called Polychromatic RBCs. Iron deficiency is the primary cause of hypochromia, and hyperchromatic is seen in sickle cell disease. Macrocytes in severe liver disease and Thalassemia, the RBCs can also be Hyperchromatic, this combination is called Leptocytes.
Increased turnover of RBC in the bone marrow results in the presence of immature RBC in the blood, these young cells retain some remnants of RNA and appear bluish when stained and laid out as a fine network called Reticulocytes. In normal conditions, the reticulocyte count is between 0.5 and 2 %. Reticulocytes over 2 % are seen in acute hemolytic anemia, massive hemorrhage, and in high altitude visitors.
When bone marrow is infiltrated, as in cancer metastasis and leukemia, Nucleated RBCs are visible in the blood and are called Erythroblasts. In times of stress, the bone marrow also releases nucleated RBCs, e.g., hypoxemia, and removal of the spleen.
Inclusion Bodies:
Inclusion bodies are iron pigment, hemoglobin, remnants of DNA and RNA fragments in the red cell cytoplasm. Inclusion bodies are called Basophilic Striplings and Howell jolly bodies.
Basophilic stippling. These inclusion bodies represent defects in hemoglobin synthesis, appear as bluish stripes, widely distributed throughout the cell cytoplasm. Examples – Megaloblastic anemia, Post splenectomy and sideroblastic anemia.
Howell Jolly bodies. These bodies appear in the periphery of the cell as purple round dots when stained with Romanowsky stain due to the presence of fragments of DNA.
Siderotic granules. These granules are iron, which remains in hemoglobin and stains blue. Example: Sideroblastic anemia.
Parasites.
The malaria parasite belongs to the Plasmodium group. Several species of Plasmodium infect humans - mostly in people living in Sub-Saharan Africa and Southeastern Asia. As there are different species, several parasitic forms, like gametocytes, schizonts and trophozoites, are also seen in the blood of patients infected with malaria. Considerable experience is required to identify these intracellular malaria parasites.
Babesiosis. Babesia infection is seen in the New England States in summer months when tics are active. The parasites appear as ring forms, often in groups, and in heavy infestation rings in groups appear outside the red cells also.
Important Points:
To a casual reader, this article may appear confusing and overlapping.
In clinical practice, however, the information is neatly and concisely presented. A few samples are presented.
Iron deficiency anemia.
Iron deficiency produces Hypochromic, Microcytic anemia. Besides a low hemoglobin, HCT (hematocrit), MCV (means corpuscular volume), MCH (mean corpuscular hemoglobin), Color index and Saturation Index are all low. RWD (red cell width distribution) is more than 15 %. This RWD finding is helpful to separate iron deficiency anemia from Thalassemia where RWD remains normal.
Macrocytic anemia.
A combination of low hemoglobin and low HCT in the presence of High MVH and MCHC (mean corpuscular hemoglobin concentration) is the rule.
Hemolytic anemia.
Intravascular hemolysis is a vast subject as such. Features of hemolytic anemia is the presence of normocytic and normochromic anemia with a normal RWD. If the hemolysis is less severe but recurrent then RWD rises above normal.
Sickle cell disease (SCD). In Benin, Senegal, and CAR (in sub-Saharan countries) death due to childhood malaria caused havoc. A mutation of the Beta Chain of the hemoglobin molecule at position 6 - substitution of amino acid glutamine to valine proved to be a lifesaver. That advantage led to a wide distribution of the mutated gene in the population. However, as people moved to the USA and Caribbean States from sub-Saharan Africa, that mutation has become a fatal mistake. In a low oxygen environment, the RBC of SCD patients changes from a disc to sickle form and obstructs blood flow in the capillaries and results in severe pain and loss of function. This results in death of cells, seen from the bone marrow to the brain.
Blood film in Sickle disease.
Thalassemia.
A growing embryo in the mother's womb draws oxygen, due to the special characteristic of Fetal Hemoglobin. If fetal hemoglobin persists in postnatal life, due to a gene mutation, it is called Thalassemia. Thalassemic patients have anemia which has the following characteristics - Microcytic, hypochromic anemia with a high RBC count, normal MCV, normal RWD, high reticulocyte count, basophilic striplings and Target cells.
Peripheral blood film in Thalassemia.
TTP (thrombotic thrombocytopenic purpura).
TTP is due to widespread platelet thrombosis in all organs producing an alarming medical situation. Hemolytic anemia due to mechanical break of RBC in their attempt to move forward in capillaries partially blocked by platelet thrombi, and a very low platelet count (10,000), the presence of schistocytes are characteristic features. Direct examination of blood film by hematologists can make a quick diagnosis.
A blood slide in TTP, the helmet cells are marked by blue