Neurotransmitters
PKGhatak, MD
Nerve cells communicate with other nerve cells, muscles, and glands, or internal organs by chemical molecules. Even though the nerve impulse travels along the nerve fibers as an electrical impulse, at the end of the nerve terminal, a tiny gap exists, that gap is bridged by a neurotransmitter,
Neurotransmitters (NT) are chemical messengers that carry forward electrical signal from neurons to postsynaptic neurons or cells of the target organ and produce the intended action. NT must meet the following criteria. NT must be synthesized by the neuron, found in the presynaptic nerve terminal, must produce depolarization and propagation of the nerve impulse. NT must be quickly removed either by enzymatic degradation, diffusion or reuptake by the nerve terminal.
From the time the first neurotransmitter (NT) Acetylcholine was discovered in 1921 by Otto Loewi of Germany, many more NTs have been added and today well over 100 NTs are known. Not all chemicals fulfill all the above criteria, however, all of them produce depolarization and transmission of nerve impulses. Chemically some of the NTs are simple gases like nitrous oxide (N0), carbon monoxide (CO) and complex protein molecules, like pituitary adenylate cyclades activating peptide, are included in the newer class of NT.
In this review, only those NTs abnormality that produces significant changes in the body are discussed. These are-
1. Acetylcholine, and Biological amines, 2. Epinephrine, 3. Noradrenaline, 4. DOPA and 5. Serotonin.
Inhibitory neurotransmitter – 6. Gamma-aminobutyric acid (GABA) and 7. Histamine.
1. Acetylcholine (ACh)
Acetylcholine is released at synaptic junctions by the neurons of the central nervous system, as shown in the diagram.
Chemistry of ACh.
ACh is synthesized from Acetyl CoA and Choline. Acetyl CoA is the end product of glucose metabolism; choline is either locally produced by the nerve cells from another amino acid serine or taken up from the blood. Chemically, choline is a Quaternary ammonium compound, acts almost like a vitamin in humans, except that it can be obtained from another amino acid. Eggs, organ meat, fish, milk and beans are good dietary sources of choline. Excess choline can cause low BP, weakness, increased sweating, fishy body odor, liver disease and cardiac problems. A deficiency of choline causes non-alcoholic fatty liver, muscle damage and hyperhomocysteinemia (high Homocysteine blood level).
Neurons take up free choline via the 1.Na+/Choline transporter,2. a degradation product of ACh by the enzyme Acetylcholinesterase from the synaptic cleft and, 3. also from blood as shown in the diagram below.
Synthesis of ACh.
Acetyl CoA + Choline = Acetylcholine, by the enzymatic action of acetylcholine-transferase.
Degradation of ACh into Acetyl CoA and Choline by enzyme Acetylcholine esterase.
Action of ACh.
Autonomic nervous system.
(a). Parasympathetic division. It acts both on ganglia and postganglionic endings and its effects are -
Eyes - Constriction of pupils and fall of intraocular pressure.
Glands - Increases secretion of GI glands,
Bronchi- Constriction of bronchi, increased mucus secretion.
Smooth muscles of GI tract – increased motility, spasm and colicky pain, contraction of gall bladder and defecation.
Heart and arterioles. Slowing of the heart rate and vasodilation of arterioles.
Urinary bladder. Precipitate micturition.
(b). Sympathetic Division - It acts only on the sympathetic ganglia and the Adrenal medulla and causes high BP and increased heart rate.
Central Nervous system. It causes restlessness, insomnia, tremors, dysarthria and convulsions.
Voluntary muscles. Contraction of muscles and fasciculation.
ACh has Nicotinic and Muscarine effects. Nicotinic receptors stimulate the ganglia of both sympathetic and parasympathetic divisions and the adrenal medulla. It also stimulates parasympathetic postganglionic nerve terminals. Nicotinic receptors stimulate the Neuromuscular junction of the skeletal muscles.
Muscarinic receptors are present in the parasympathetic nervous system and signal secretion from glands and smooth muscle contractions. Muscarine has no action on the skeletal muscles and does not act on the brain cells.
Diseases, due to autoimmune disease and some unknown causes, decrease the functions of ACh: these conditions are - Myasthenia gravis, Eaton Lambert syndrome, Guillain-Barre syndrome and Ascending paralysis in febrile children.
When used as a drug - it temporarily produces muscle paralysis and is used every day in surgery to ensure a better surgical outcome. Patients on mechanical ventilators at times require muscle paralytic drugs to prevent patients from struggling to breathe.
2. Biological amines:
Walter Bradford Cannon of Massachusetts, USA, in 1932 discussed the properties of adrenaline and used this phrase - Flight or Flight response.
Epinephrine and Noradrenaline.
In Europe, these two neurotransmitters are known as Adrenaline and Noradrenaline. Both Adrenaline and Noradrenaline are hormones. Norepinephrine (noradrenaline) is the neurotransmitter of the sympathetic division of the autonomic nervous system.
Biosynthesis of Norepinephrine.
L-Phenylalanine, an amino acid, is the source of Dopamine and Epinephrine, the intermediate steps and enzymes involved in this process are as follows.
L-Phenylalanine to L-Tyrosine by enzyme Amino acid Hydroxylase.
L-Tyrosine to L-Dopa. (1-3,4 -Dihydroxyphenylalanine) by the enzyme amino acid Hydroxylase.
L- Dopamine to Norepinephrine by enzyme Betahydroxylase.
Norepinephrine to Epinephrine by the enzyme N-Methyltransferase.
Noradrenaline is the transmitter for all the neurons of the brain and spinal cord of the sympathetic division of CNS, and outside the CNS, for the sympathetic postganglionic neurons. Noradrenaline increases blood pressure vessels due to increased tone. It produces bronchodilatation in the airways of the lungs and relieves nasal congestion. The difference in action is based on alpha and beta receptors and their subtypes.
Origin of noradrenergic neuron.
These neurons originate from the locus coeruleus, tegmentum and dorsal medullary group.
Action of Noradrenaline and Epinephrine
|
Effect on |
Norepinephrine |
Epinephrine |
|
Heart rate. |
Slowed |
increased |
|
Force of cardiac contraction |
No effect |
increased |
|
Cardiac output |
No effect |
increased |
|
Cardiac irritability |
increased |
Much increased |
|
Systolic BP |
Rises |
rises |
|
Diastolic |
Rises |
falls |
|
Vascular bed in muscles |
constriction |
dilatation |
|
Vascular bed skin & viscera |
contraction |
contraction |
|
Vascular resistance in the heart |
increased |
decreased |
|
Glucose metabolism |
unchanged |
increased |
|
Bronchial smooth muscles |
No effect |
relaxed |
|
Intestinal muscles |
relaxation |
relaxation |
|
Intestinal sphincters |
constriction |
relaxation |
|
Pregnant uterus |
Increased contractions |
Contraction lessened |
|
Capillary permeability |
No effect |
reduced |
|
|
|
|
|
|
|
|
Epinephrine is a lifesaving drug in an acute allergic reaction and anaphylactic shock producing laryngeal edema and death due to airway obstruction. Adrenaline has multiple applications in everyday medical practice and is too numerous to list here.
3. Serotonin.
Serotonin chemically is 5-Hydroxytryptamine (5lHT). It is formed from the amino acid Tryptophan to 5-Hydroxytryptophan by enzyme Trytophanhydoxylase (adding “OH” group) and then to 5-Hydroxytryptophan (serotonin) by enzyme Aromatic amino acid decarboxylase and coenzyme pyridoxal phosphate (removing COOH group). 5-HT is present in large amounts in the GI tract and the brain neurons and platelets.
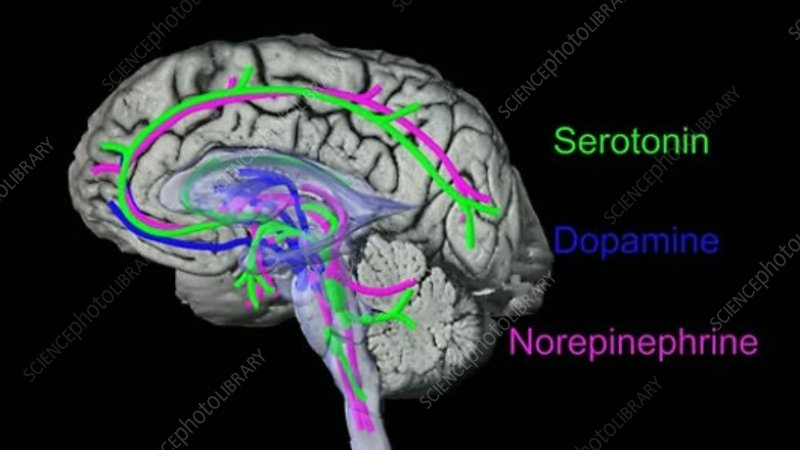
Serotonin acts on the areas of the brain and is shown in green color in the diagram below.
Serotonin is the neurotransmitter for appetite, sleep, memory, happiness, mood, vomiting center, sexual arousal and body temperature maintenance by its actions on the forebrain, brainstem and cerebellum. Lack of serotonin produces depression, anxiety and other psychological dysfunctions.
Serotonin receptor.
Serotonin (5-HT) receptors are designated by digits 1 to 7 and the receptors of 5-HT1 are assigned - A to F. The receptors of 5-HT 2 have A to C subtypes. The action of serotonin varies according to its binding with the type of receptor.
5-HT1A is mostly related to mood, learning, memory and behavior.
5-HT1B produces vasoconstriction. 5-HT2 signals via activation of phospholipase.
5-HT2A stimulates urinary bladder contraction.
5-HT2B increases pulmonary hypertension. and in general, produces inhibitory actions and opposes 5-HT1A effects.
5-HT2C stimulates appetite.
5-HT3 can produce nausea and vomiting.
5-HT4 increases GI motility.
5-HT5 consolidates memory.
5-HT6 increases depressive mood.
5-HT7 opposes 5-HT6 effects on mood.
Location of Serotonin receptors in the brain.
The Raphe nuclei B1 to B9 are serotonergic. These neurons are most abundant in the reticular formation, the axons of these neurons connect the brain and spinal cord nuclei.
Serotonin has a dominant role in understanding psychiatric disorders and depression. Therapeutic drugs are used extensively to increase the concentration or prolongation of the action of serotonin in the synaptic cleft.
4. Dopamine.
Dopamine is primarily an inhibitory neurotransmitter, which controls agitation and excessive motor actions.
Biosynthesis of L-DOPA (L-dihydroxyphenylalanine).
Biosynthesis is mentioned earlier. DOPA, norepinephrine and epinephrine are collectively known as Catecholamines. L-DOPA can enter the brain but L-Dopamine is blocked by the blood-brain barrier. In the brain, L-DOPA is converted to L-Dopamine by decarboxylate and Vitamin B6 as a cofactor. This actions take place in Sustantia Niagra. After dopamine is release at the nerve terminals, it is quickly broken down by catechol methyl-O- transferase.
Dopamine receptors and action.
|
Receptor subfamily |
Location |
Action |
Therapeutic potential |
|
Central |
|||
|
D1 and D2 |
substantia nigra and striatum |
motor control |
agonists - Parkinson's disease |
|
D1 and D2 |
limbic cortex and associated structures |
information processing |
antagonists - schizophrenia |
|
D2 |
anterior pituitary |
inhibits prolactin release |
agonists - hyper-prolactinemia |
|
Peripheral |
|||
|
D1 |
blood vessels |
vasodilatation |
agonists - congestive |
|
D1 |
proximal tubule cells |
natriuresis |
heart failure |
|
D2 |
sympathetic nerve terminals |
decreases release |
hypertension |
Dopamine has both CNS and outside CNS effects.
In the brain, dopamine edits signals that are going out to the skeletal muscle. In the limbic system, it organizes and forms emotional memory in associated mood elevation.
Outside the CNS, Dopamine is produced locally and acts locally (action is called paracrine effects). Dopamine increases heart rate and BP. It is suspected that Primary Hypertension is due to an abnormal dopamine action on the kidneys. In the pancreas, it decreases insulin production, on the GI tract, decreases motility, acts to protect the GI mucosa and boosts local cellular immunity. It appears that dopamine acts as a natriuretic hormone in the kidneys.
Diseases involving movement disorders, like Parkinson's disease, Restless leg syndrome and minor strokes, are treated with DOPA.
5. Gamma Amino butyric acid (GABA).
GABA is derived from Glutamate. Both Glutamate and GABA are neurotransmitters of the central nervous system. Glutamate is a neuroexciter and is widely distributed in the brain, mostly in small sized neurons. GABA is an inhibitor NT. GABA neurons are present in the Limbic area of the brain, from these nuclei GABA connects many areas of the brain. A diagram below shows the areas of influence of GABA.
Chemistry:
Brain neurons produce GABA from glutamine by decarboxylation by the enzyme decarboxylase. The reaction is a rate limiting reaction. GABA concentration in the brain is high.
Mechanism of action of GABA:
GABA has two isoforms, Ionotropic (GABA A) and metabotropic (GABA B) forms. Two separate genes on two chromosomes encode the production of isoforms. GABA has two metabolites, Homocarnosine and pyrrolidinone and both these chemicals are anticonvulsants. GABA prevents hyperpolarization and reduces incoming and outgoing signal strength. GABA A receptors are present all throughout the brain. GABA B receptors are formed by the fusion of two G-protein molecules.
Blood-brain barrier prevents GABA from entering the brain but Glutamine is free to enter. Food containing glutamine is soybean, brown rice, chestnut, mushroom, tomato, spinach, cabbage and cauliflower.
Fluctuation of the levels of GABA has been linked with Autism, Parkinson's disease and anxiety.
Therapeutic drugs having GABA-like action are used as pain control medication but the therapeutic action of these medicines does not match the theoretical possibilities it promises.
6. Histamine.
Histamine is well known as a mediator of allergic reactions. It is present in the mast cells of the skin and in the basophils of blood. It enhances inflammatory reactions by increasing vascular permeability and the production of mucus.
As an NT is not that well known. In the brain, it acts via H1, H2 and H3 receptors.
Action in the brain results in wakefulness, alertness and quickens reaction time.
Distribution of Histamine containing cells.
In CNS: Hypothalamic region of the brain.
Outside the brain: The nose, mouth, feet, skin, and feet have a good number of mast cells. In the stomach, chromaffin cells produce and release histamine.
Chemistry: Histamine is produced from the amino acid Histidine by the enzyme histidine decarboxylase.
Enzyme histidine N-methyltransferase and diamine oxidase degrade histamine.
Receptors. Histamine receptors are H1 to H4.
H1 receptors. Dendrons (short arms of neurons) of the Tuberomammillary nucleus terminate in the dorsal raphe and locus coeruleus. These cells regulate sleep-wakefulness cycles, body temperature, appetite, coordinate endocrine hormones and cognition.
H2 receptors. Basal ganglia, hippocampus and dentate nucleus have histamine 2 receptors. Modification of motor activities is the main function. In the stomach, H2 receptors on the parietal cells are activated and histamine increases HCl acid production.
H3 receptors. The precise location is not worked out. The action appears to counteract acetylcholine, serotonin and norepinephrine actions.
H4 receptors. H4 receptors in the brain have not been detected.
The realm of antihistamine drugs is increasing with new discoveries of histamine receptors and their role in the etiology of diseases.
8. Other NTs.
Glycine.
Glycine is an amino acid, present in every living cell and besides performing metabolic functions, it also acts as a neurotransmitter for incoming somatic sensations like pain and touch, vision and auditory sensation. Glycine also acts on strychnine-sensitive receptors and produces inhibitory action and modulates excitatory neurotransmission of glutamine in glial cells.
The final word.
Neurotransmitters are chemical messengers synthesized by neurons and delivered at the synaptic cleft in order to ferry the nerve impulse to the next neuron or to target cells. In the cerebral cortex, the prime NT is acetylcholine. In the autonomic nervous system, ACh is also the sole NT for both parasympathetic ganglia and postganglionic nerve terminals. In the sympathetic nervous system, ACh is NT for the sympathetic ganglia but epinephrine is the prime NT for postganglionic nerve terminals. In the Limbic nervous system, multiple NTs interact, modify, enhance, or inhibit nerve impulses.
NTs are also classified as excitatory or inhibitory. The same NT may act as both excitatory and inhibitory depending on the receptor it binds. The molecular structure of NT must fit with receptors like pieces of Logo fit with another - a Levo (l) or Dextro (d) from; an aliphatic chain or ring form, makes that difference. And finally, even minor NTs have major effects on the body.
************************************