Dracunculiasis
Guinea worm Disease
PKGhatak, MD
Guinea worm disease and the name of President Jimmy Carter are intertwined, to recall one, the other name pops up immediately. President Jimmy Carter single-handedly brought the misery of African people suffering from Guinea worm disease to our consciousness.
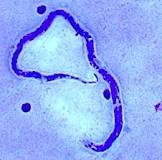
Dracunculus medinences, the parasitic nematode (roundworm) has been a curse of humanity known since 1000 BCE. The worm lives a symbiotic life with the water fleas called Copepods, which are abundant in the small pools of water in Sub-Saharan Africa. Farmers and others drink water from these pools during hot summer months and ingest Copepods and become infected with the Guinea worm larva.
Life cycle of Dracunculus medinences:
Humans, domesticated dogs, and cattle are victims of the roundworm. Dogs and cattle are infected because of their closeness with their masters. People develop incessant burning pain during the release of larvae by the gravid female. Farmers dip their feet in the pool in order to get some relief from the burning sensation. The worm releases thousands of larvae, which are food for the Copepods.
Thirsty men drink water from the pool during summer days, working in their fields under the hot sun. The outer cuticle of the copepods dissolves by the gastric juices. The released larvae enter the small intestine and begin to move along the tissue planes to the abdominal and thoracic muscles. In about 3 months, the worms reach sexual maturity. There, the male and female worms mate, and soon the male worm dies. The female starts her migration towards inferior extremities and finally settles underneath the skin of one leg. It takes 12 to 14 months to complete this migration. Once the right moment arises, the worm breaks through the skin of the foot or lower leg, forming an ulcer, and continues to deliver larvae for 10 weeks.
The victim suffers burning pain during the entire period. There are no medications to kill the worm or any vaccine to prevent infection. The only solution, as President Carter saw, was to provide people with simple water filters and educate, educate and educate people on how to protect themselves. And he nearly achieved his goal.
Guinea worm diseases:
Nausea, vomiting, and diarrhea following drinking contaminated water are common.
Painful blisters on the legs, leg ulcers, secondary bacterial infection, draining wounds, abscesses, and gangrene of limbs are similar symptoms in all the villagers.
About 1 % fatality from septicemia.
Control of Guinea worm:
This task is a WHO project.
People at risk of Guinea worm infestation:
People living in the countries located in sub-Saharan Africa from Angola to South Sudan are at risk.
The success story:
In 1986, 3.5 million people had draculiasis and in 2022 only 13 people were found with guinea worm disease. 17 counties out of 21 were free of guinea worm. That is a 99.99 % success rate.
Treatment :
No improvement has taken place over the age-old custom of grabbing the worm with a tweezer, as it breaks the skin. Tie the worm to a small stick and periodically twist the stick with the worm. Slowly and bit by bit, the entire I meter long and 1 to 2 mm wide Drancanculia will be out of the leg. But multiple worm infestations are the norm, and so the misery of the sufferers continues.
The name Drancunculus is a misnomer, the worm does not drink blood like Dracula or another worm – Hookworm.
***********************************************************************