Malaria
Some important aspects
PKGhatak, MD
A tiny one-cell parasite infected primates in equatorial Africa, perhaps thousands of years ago. At a later date, the parasite found humans as suitable prey. It was a time before writing developed. We do not know whether those people knew malaria was a parasitic disease. Egyptian, Chinese and Indian physicians left some documents. After a retrospective analysis of those documents, some appeared to be malaria fever cases.
Romans thought the febrile illness was from Mal-Aria (bad air) rising from the swamps; they correctly identified the swamp as the breeding ground of mosquitoes but failed to connect the mosquitoes with the spread of malaria.
That task was completed in 1857 in Kolkata, India by Ronald Ross. He identified the parasite in the female Anopheles mosquitoes. He recovered the same parasite Plasmodium relictum from the blood of birds, linking mosquitoes with birds' malaria. He was awarded the Nobel Prize in 1902 for his groundbreaking research. Subsequently, other researchers discovered the complete life cycle of the malaria parasite - the Plasmodium.
Malaria parasite.
Malaria belongs to the Genus Plasmodium of the Superphylum Alveolate, and the Phylum Apicomplexa. Like all Alveolate, Plasmodium contains a plant plasmid, used in Photosynthesis by the plant. The plasmodial plasmid is a bit different, it is used in extracting a fatty acid, Isoprenoid, from the host cells in order to develop and multiply in the liver and RBCs in humans and in the salivary gland of mosquitoes, and not used in photosynthesis.
Six species of Plasmodium infect humans, namely -
1.Plasmodium falciparum (P. falciparum)
2. P. malariae
3. P. vivax (with identical morphologically P. simiovale and two other related species P. minuta and P. tenue)
4.P. ovale
5. P. Knowles.
Know the Female Mosquitoes.
Female Mosquitoes are equipped with chemical sensors for Carboxylic acid, a CO2 derivative. Using the sensors, mosquitoes zero in on a person who has higher carboxylic acid in the breath. Female mosquitoes must have a high protein meal (blood) for the development of eggs and laying fertilized eggs on the surface of non-flowing bodies of water, e.g., ponds/swamps, etc.
Follow the parasite.
Mosquitoes' salivary glands are loaded with the infective forms of the parasite, and mosquitoes deposit them when they bite and suck human blood. At this stage, the parasite is known as Schizont (no English word for it). From the skin, the parasites travel to the liver and enter the liver cells. In the hepatocytes (liver cells) the parasite multiplies. The parasites break free from the liver cells and infect RBCs. Duffy antigen receptors on the RBC surface are the anchoring point of the parasite and serve as the entry point into the red cells. At this stage, the parasite is called Merozoites. In the RBCs, the parasites begin to divide by themselves (nonsexual multiplication) and the new Merozoites very quickly multiply and reach a huge number and the red cells burst open and the merozoites enter into the bloodstream and begin to infect more RBCs. And the cycle keeps repeating until some merozoites change to male and female reproductive units called Gametocytes and wait for the mosquito to bite and draw blood. In the gut of the mosquito, the male and female gametocytes unite and produce their progeny, the schizonts. Schizonts move to salivary glands and wait to infect a new victim.
Time taken for the parasite to complete human RBC cycles.
In the case of P. falciparum, P. ovale and P. vivax the cycle is repeated every 3 days. In P. knowlesi and P. malariae the cycle only a day.
Symptoms of malaria.
Malaria symptoms vary according to the species of Plasmodium.
a. Shaking chills followed by high fever.
With no warning, a sudden onset of chills and shaking starts. The chattering of teeth, assuming a fetal position and covering the body with all comforters or blankets does not bring any relief of chills till the fever starts. The temperature is usually 104 degrees or higher and weakens, profuse sweating and prostration follow when the fever breaks.
b. Hemolytic anemia, jaundice and renal insufficiency and renal failure.
The broken RBCs release not only the parasites but also the hemoglobin into circulation. Free hemoglobin is an oxidant that damages glomerular capillary endothelium and decreases renal filtration. In recurrent episodes of hemolytic anemia, renal failure develops. Hemoglobin is broken down in the liver into heme and globulin. The heme is a waste product. Light jaundice becomes evident, urine and stool develop darker shades of yellow.
c. Anemia, failure of children to thrive in endemic areas, susceptibility to tuberculosis and HIV infections are common in certain countries in alarming numbers.
d. Enlarged spleen and liver and marked anemia. Parasites induce immune reactions and chronic inflammation and enlargement of organs.
e. Blackwater fever.
Certain patients, generally non-native residents, taking Quinne irregularly for the treatment of malaria develop dark colored urine due to the presence of hemoglobin in urine and chronic renal failure. It is thought to be an autoimmune disease, triggered by the interaction of quinine with plasmodium. The antibodies then attack the kidneys.
Laboratory diagnosis:
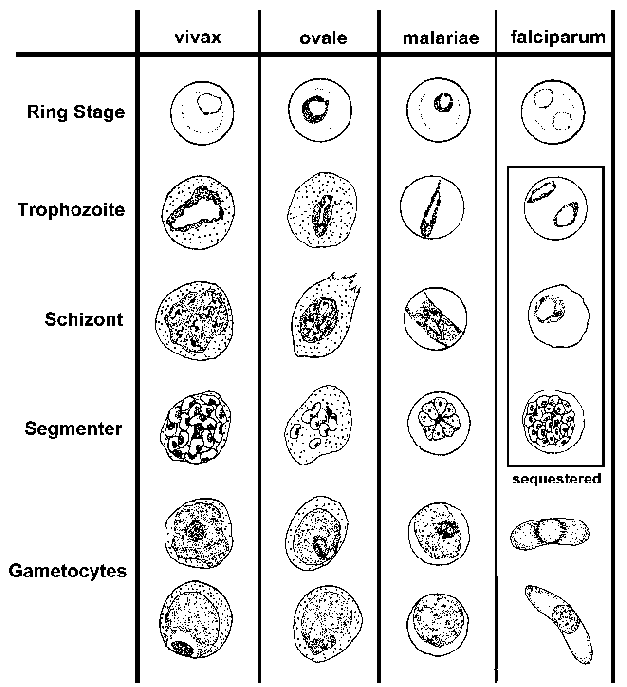
Peripheral blood examination.
Until the use of direct detection of the antigen of the malaria species by PCR was introduced, the microscopic examination of blood slides for the presence of parasites was the accepted method of diagnosis of malaria.
|
|
|
|
Special features of falciparum malaria.
P. falciparum fever is also called malignant malaria and cerebral malaria. Worldwide, 2 million people are infected and ½ million die on yearly basis. The initial symptoms marked by shaking chills last only 30 min, followed by high fever, headaches, and confusion and children develop convulsions and coma rapidly. The fever returns every 48 hrs. Falciparum induces swelling of the RBCs, and the surface membrane protein of the parasite changes to knob like projections and attaches to the endothelium of capillaries. The circulation is compromised and endothelial cell hypoxia induces adhesive properties of the endothelial cells and locally released cytokines, cells facilitate platelet thrombi and the microcirculation of the tissue is cut off. Hypoxic injury of the brain occurs in the basal ganglia and hindbrain. Generalized swelling of the brain produces encephalopathy and various degrees of coma and convulsions. With early medical intervention, cerebral changes are reversible. The mechanism of acute renal injury is multiple. Free hemoglobin in the circulation oxidizes glomerular capillaries, swelling, edema and piecemeal necrosis of uneven distribution of renal lesions leads to a marked reduction of GFR. The capillary circulation of the renal tubules is severely compromised and results in Acute Tubular Necrosis and renal failure. Nearly 40 % of adults develop renal failure and cerebral malaria incidence is high in children and the mortality is high.
P. vivax.
Vivax malaria is less virulent than falciparum but deaths are still very high. Currently, southern Africa, Central & South American countries, the Indian continent, and Indonesia & Malaysia peninsular regions report most cases. Fever recurs every 48 hours, the temperature reaches 104F, and the febrile period is about 4-8 hours. Most of the symptoms are from released cytokines, TNF alpha and IL-6. Pulmonary involvement and enlarged spleen often rupture without trauma. Anemia is of chronic nature and secondary infections in endemic areas are not unusual. The parasite may remain dormant in the liver for years and one infection triggers six or more infections. In addition to renal failure, hypoglycemia, low platelet count and bleeding episode, loss of taste and occasionally lack of fever are some of the unusual features.
P. ovale.
Ovale malaria is the mildest form of human malaria. It is seen in the Indian subcontinent. The fever recurs every 48 hours (tertian fever). Fever begins after 12 days following mosquito bites.
P. malariae. Massive splenomegaly from the abnormal immune response is a feature of P. malariae malaria. Fever recurs every 48 hours intervals. The incubation period is 16 to 60 days. Nephrotic syndrome is due to immune complex formation with malaria antigen and antibody and produces renal failure.
P. Knowles. It is the malaria of Macaque monkeys; humans acquire malaria due to close contact with macaques. Fever recurs every day (quotidian fever). GI symptoms like hiccups and dysphagia are distinguishing symptoms. Because of a few cases in the community, robust immunity does not develop. So, the fever continues and results in anemia and weakness.
Asymptomatic Carrier.
In endemic area, some people acquire immunity from repeated malaria infections. Unless their immunity is compromised by intercurrent infections or diseases, they remain malaria free. Once they move to other countries where malaria is rare, they can transmit the parasite to others by donating blood or organs.
Malaria continually develops resistance to drugs.
Plasmodium quickly develops gene mutations and renders drugs ineffective. For example, anti-folate medication becomes ineffective due to a point mutation of the Dihydrofolate dehydrogenase enzyme. Another point mutation involving two transporter proteins. By accruing mutations, the parasite increases the rate of expulsion of antimalarial drugs from the cytosol. Still, another way to develop drug resistance is by gene amplification of those genes mentioned above, making the mechanism work at a higher level, making unmatched therapeutic blood levels.
Defects in the DNA repair genes accelerate mutations, specially in P. falciparum.
Anti-malaria drugs.
Currently 5 groups of antimalarial drugs are available to treat malaria.
1. Endoperoxide – example Artemisinin.
2. 4-Aminoquinolines and related derivatives – Chloroquine, Mefloquine.
3. Napthaquinolies – atovaquone.
4. Antifolate – Pyrimethionine.
5. 8-Aminiquinols – Primaquine.
P. falciparum has developed resistance to every one of the above 5 groups of drugs.
Secondary drugs used in conjunction with the above 5 groups are -
Doxycyclines, Sulfadoxime, Lumefantrine.
New class of Drugs.
Monoclonal antibodies are used subcutaneously, prevent schizonts from attaching to RBCs and subsequently infect liver cells when used in combination with other standard antimalarials. Imatinib, a small molecule anti-leukemia drug, works by inhibiting the Kinase, has also been used recently and has the potential to rapidly clear malaria parasites from blood and liver. A drug, Alisporivir, used in hepatitis C, was found to be effective in Artemisinin-resistant P. falciparum infection.
Several drugs are used in various combinations like chemotherapy for cancer. WHO's recommendations of drug therapy and chemoprophylaxis are essential to keep informed about the therapeutic challenges posed by rapid drug-resistant malaria spreading from one region to the other endemic area.
wormwoodChinese sweet wormwood, source of artemisinin.
Artemisinin was introduced by Dr.Tu Youyou in the western world, at one time Artemisinin was the mainstay of drug therapy of P. falciparum and was used extensively alone or in many various combinations with other compounds. For his work, he too received the Nobel prize in 2015.
Malaria therapy for neurosyphilis.
Before Penicillin was available to treat syphilis, fever by P. vivax infection induced fever as the therapy for neurosyphilis by introduced by Julius Wagner-Jauregg. In Europe P. knowles was used for this malaria therapy till 1950. For this therapy, he was awarded the Nobel prize in medicine in 1972.
*****************************



No comments:
Post a Comment