Cornea and Cornea Transplant
PKGhatak, MD
Eye to
eye contact is an essential characteristic of humans. It is said one
can see the soul of a person looking through the eyes of others. Medical
science has not advanced to that level to know where the soul resides,
but what a person sees looking directly into the eyes of the other is a colored iris within which is a central beautiful transparent zone,
the dept of that remains elusive, probably the source of the idea of the location of the human soul. That central transparent zone is the pupil of the eyes, a part of the Cornea.
Parts
of the cornea.
Eyes
are extensions of the central nervous system and develop at the same
time as the brain is taking shape. The outermost layer of the eye is made
up of tough collagen tissue, the white of the eyes is called the sclera and the transparent part is the cornea. The main function of the sclera is to protect the inner delicate eye structures and prevent infection. The function of the cornea is to bring objects in focus on the retina for vision. Cornea
is one of a few immune privileged tissues, which are out of reach of
immune surveillance cells and immune directed inflammation. Others
such as tissue/organs are the placenta, fetus, sperm and articular
cartilage.
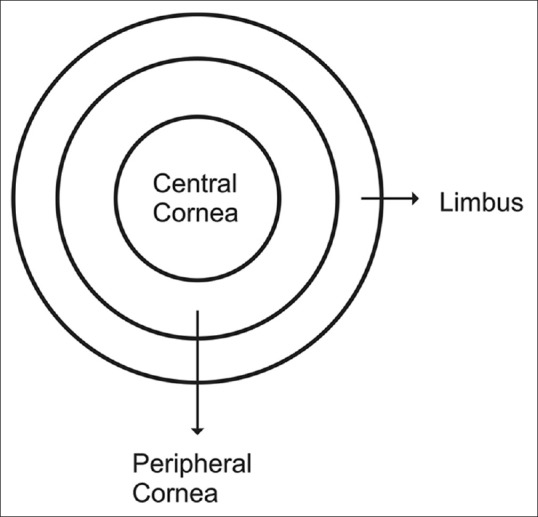
Anatomy
and the property of the cornea.
The
cornea is 11 to 12 mm in diameter, the thickness varies from 0.5 mm
in the center to 0.8 mm at the periphery. The cornea is devoid of blood
vessels and lymphatic channels.
Histology of cornea.
Cornea
from outside to inside.Epithelium.
This
layer of non-keratinized stratified epithelium consists of 6 layers
of cells. The epithelium of the cornea is continuous with the conjunctiva of
the eye. The cells of the basal layer of epithelium have fast
regenerative capacity and quickly replace any damaged cells.
Bowman's
membrane.
It is
a tough tissue made up of collagen I fibrils, and the fibrils are
tightly interwoven and adhere to each other. Bowman's capsule is about 14 micrometers in thickness. and devoid of any cells.
Stroma.
It is
also called the substantia propria. This layer is made of regularly
arranged collagen fibrils of type I collagen, arranged in thin sheets
like pages of a book and has 200 layers. In this stoma, a few
scattered but interconnected keratinocyte cells are present, these cells are responsible for the daily maintenance and repair of the stroma.
Descemet's
membrane.
This
layer is also called the posterior limiting membrane. It is 10 micrometers thick and made up of collagen IV fibrils. The thickness of Descemet's
membrane increases with age and can be 20 micrometers in thickness. A
tough layer of the innermost part of Descemet's membrane is known as the Dua layer, which is about 15 micrometers in thickness but can withstand
2 bars of pressure.
Endothelium.
Anatomically, the term endothelium is appropriate but these cells do not come in
contact with blood. The endothelium is only one layer of cells, 5
micrometers in thickness, and the cells contain a large number of
mitochondria. These cells are bathed in aqueous humor and regulate a
proper fluid balance of the cornea. The endothelium cannot regenerate. When
one cell dies, the adjoining cells stretch to cover
the empty space. When a significant loss of cells happens, the cornea
swells and becomes opaque and vision falls.
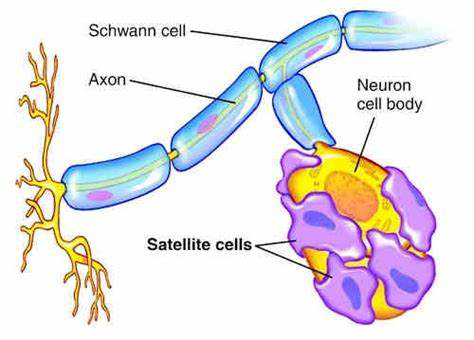
Nerve
supply.
The cornea is innervated by sensory fibers of the ophthalmic division of the trigeminal
nerve. Unmedullated fibers are very sensitive and carry pain
sensation. The pain receptors of the cornea are 500 times greater than the skin and any corneal injury is excruciatingly painful.
The
nerve terminals enter the cornea through three sites – at the episclera,
sclera and conjunctiva. The nerve fibers form a network in three levels
-midstromal, subbasal and epithelial and from these networks, all the
structures of the eye are innervated.
Optical property of cornea.
1. Refractive
index. The cornea is highly transparent and allows 95% of daylight waves to penetrate
inside. A radial colored diaphragm, the Iris of the eye, by varying
its size of the pupil, regulates the amount of light to enter the eye. The
size of the pupil can vary between 1.5 mm to 8 mm in diameter. As
stated earlier, the cornea is composed of layers of cells of
different types, the refractive index of the epithelium, the stromal anterior
and posterior wall is 1.401. 1.38, and 1.373 respectively.
The
refractive index of the cornea, as a whole, is n = 1.3765 +/- 0.0005. (see footnote)
Diopter
of eye.
The
property of refracting light in ophthalmology is expressed as Diopter
(D). The
eye contains two focusing lenses, the cornea and the crystalline lens.
The cornea has 45 diopters and the lens 15 diopters for a combined
60 diopters of focusing power. The accommodation apparatus of the eye can
add additional diopters required for near vision.
Cornea Transplant.
In
December 1905, Edward Zirm, an Austrian ophthalmologist, was the first
person to successfully perform a cornea transplant on a human. Cornea transplants are relatively problem free because the cornea is a
privileged tissue and does not attack the transplanted cornea. Various
modifications and advances in corneal transplant, like selected
corneal layers rather than full-thickness cornea grafts, refined
sutures and the use of the surgical microscope and eye banks, have resulted in
high demand worldwide for cornea transplants. However, for every 1
successful transplant, 70 others are waiting because of the limited availability of donated cornea.
Indication
of cornea transplant.
The opacity of the cornea from any conditions and even with associated other eye conditions
amenable to medical treatment like glaucoma and cataract is
considered for a cornea transplant.
Statistics.
About
10 million people in the world are blind due to corneal diseases.
In
2012, some 46,000 people in the USA had corneal transplants; 185,000
corneal transplants were performed in 116 countries of the world in
the same year.
Eye
diseases are treated by a cornea transplant.
1. Penetrating
injury to the cornea.
2. Opacity
from corneal ulcers or wounds
3. Keratoconus.
In this condition, the cornea bulges forward due to structural
weakness.
4. Fuchs
dystrophy. It is an inherited condition acquired by dominant
inheritance. The endothelial cells begin to die out slowly, as one
cell dies, the adjoining cells stretch to cover the void. When many
cells are gone, the remaining cells form little clumps. Fluid in the stromal layer accumulates and the opacity of the cornea becomes evident.
5. Thinning
and tearing of cornea.
Types
of transplants. The
medical term for a corneal transplant is Keratoplasty.
1. Full-thickness
Keratoplasty.
In
penetrating wounds of the cornea. a full-thickness graft is best suited.
A circular portion of the damaged cornea is cut out and a graft, exactly
matching the removed portion, is transplanted and kept in place by
placing 16 sutures. In general, it takes 12 weeks for this type of
graft to be fully functional and may still be dislodged in blunt
trauma to the eye.
2. Endothelial
transplant.
Descemet's
stripping automated endothelial keratoplasty is the choice of
operation for Fuchs endothelial dystrophy and bullous keratopathy.
3. Deep
Anterior Lamellar Keratoplasty.
Conditions
like keratoconus and corneal stromal scar are suitable for this
operation.
4. Posterior
Lamellar Keratoplasty.
Corneal
opacity due to damage to the inner layers of the cornea is treated by this
method. Only the damaged layers are replaced by the same layer of tissue of the donated cornea. Technically, this operation has an advantage over a
full-thickness graft, only 2 sutures can hold the graft in place and
in 2 weeks, the graft is fully functional and the refractive power
matches with preoperative evaluation. The graft is not displaced in
blunt injury to the eye.
5. Artificial Cornea Transplant.
The
Boston K-Pro company made an artificial cornea by using medical-grade
poly-methyl-meth-acrylate (PMMA). A cornea graft tissue is encased
in two layers of PMMA. Dr. Francis Price performed the first
artificial cornea transplant in Indiana, USA in 2004.
Indication for artificial cornea graft.
1. Artificial
cornea grafts have been used successfully in cases of failed grafting on multiple previous attempts.
2. Steven Johnson syndrome.
3.Ocular cicatricial pemphigoid.
4. Systemic
autoimmune disease produces corneal opacity.
5. Ocular burns.
6. Aniridia
(absence of the iris) and other conditions.
_________________________________________________________________.
Footnote:
Refractive
Index of Cornea.
The
refractive index is the bending of light rays when entering another
medium. The refractive index varies with the wavelength of light; the rainbow is a result of this phenomenon. The diagram below shows the
angle of the entering rays at the contact surface and the angle
the refracted light makes inside the other medium. The ratio of
these two angles is known as the refractive index.
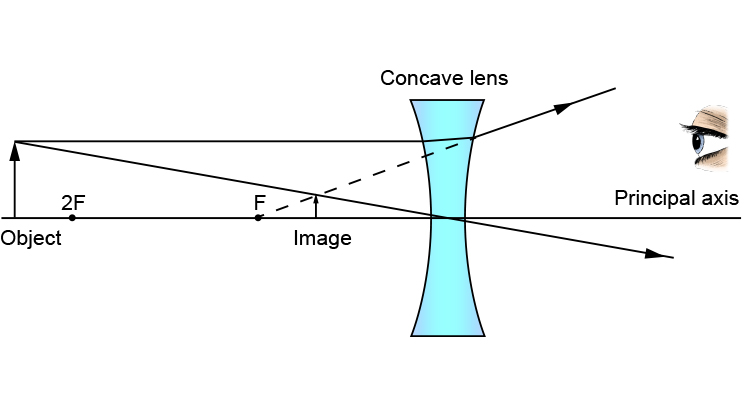
Focal Point of a lens.
The point is where parallel light rays converge into a point in the case of a convex lens.
Focal Length of a lens.
Focal length is the distance in mm from the distance from the lens to the focal point.
For a concave lens, these two definitions are the same, except in a concave lens the light rays diverge out from the parallel axis and the focal length is given in a negative value.
Diopter.
In
medicine, the focal length of the cornea or the crystalline lens is
expressed as Diopter (D). It is the reciprocal of the focal length of the lens expressed in meters. 1D
is equal = 1m – 1. or, 1000/ focal length of the lens in mm. If
additional eyeglasses are required for clear vision, the
prescription is written + D for correction of
far vision, and - D for correction of near vision. The patient is said to have near vision when the image falls in front of the fovea centralis (used for reading) of the retina and a negative D lens will make the image on the fovea centralis. For patients with far vision, the reverse is true and for correction, a positive value D lens is needed.
The diagram shows the difference between convex and concave lenses.
Converging lens (+D)

Diverging lens (-D)
Additional graph representing a concave lens forming an image.
***************************************************************