How we see the outside world.
The science behind it.
PKGhatak, MD
Looking straight ahead, we see a vast area, horizon to horizon. Using a visual field measurement chart and recording one eye at a time, we find each eye has a visual field of 155 degrees on the horizontal plane and 130 degrees on the vertical plane. By adding the visual fields of two eyes together, our visual field should be 310 degrees but in fact, the visual field is smaller because the nasal field of the two eyes overlaps.
That overlap gives us the dept of vision, meaning, we can judge the distance of an object in front. It is an essential quality for reading, writing, driving, painting, target shooting and other activities which require bringing objects in sharp focus.
The diagram above illustrates visual fields and where the images develop.
The visual field is divided into the Nasal field and the ear (Temporal field. To make a clear distinction between the left and right visual fields, the right-hand side of the visual field is colored red and the blue color for the left.
Note that the nerve fibers carrying the image from the nasal half of the right eye, represented by blue lines, are crossing the midline and going to the left side to join the nerve fibers carrying the image from the temporal half of the left eye. The same is true for the left eye, marked with red color.
It is interesting to note that crossed and uncrossed nerve fibers join and carry images representing the right and left visual fields and not the left or right eyes.
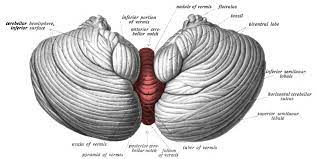
The second point to note is that the nerve fibers make a connection at a nerve center called Lateral Geniculate Body (LGB). The right visual field image goes to the left side and the left visual field image to the right side of the LGB. The stratification of nerve fibers is maintained in the LGB, meaning the temporal fibers remain outer and nasal fibers on the inner nuclei of the LGB.
The third point is that the same stratification is also maintained in the Visual Cortex. The visual cortex is located in the back of the cerebral hemisphere, one on each side in the Occipital Lobe.
Not shown in the diagram, there is upper and lower field stratification on the visual cortex. The lower half of the visual field is represented in the upper part of the opposite cortex, and the upper half in the lower visual cortex.
By knowing the detailed anatomy, the doctors are capable of detecting any segmental visual field loss and treating properly without wasting much time.
How two images merge into one.
This fusion of two images in the visual cortex and perceived as one depends on unison eye movement and convergent reflexes that make image generation on the corresponding points on each retina. When initial images are close but not exactly one, then a further adjustment is made by the eye muscles to focus properly.
Why does an object too close to the eyes appear blurred.
The eyes are situated 2 inches apart. The images of the two eyes are not precisely the same, the right eyes see a little more on the right-hand side and the left eyes see more on the left-hand side. The images fuse completely when the object is at a comfortable distance from the eyes. The disparity grows more and more when the object is brought closer and closer.
How images are formed on the retina.
Light rays travel in straight lines in all directions from an object. The pupil by changing its size brings light rays in focus on the retina. The photosensitive pigment of the retina converts the electromagnetic energy of light into electrical stimuli. Next, the rods and cones cells of the retina perceive the stimuli and then pass them to nerve cells which convert the electrical stimuli into nerve impulses and send out nerve impulses to the brain.
How the color is represented in the brain.
In the daytime, sun rays are bright but colorless. But we know that daylight hides 7 colors from red to violet (color of the rainbow) in it. The color receptors of the eyes are cone shaped cells, called cones of the retina. Cones are plentiful in the central part of the retina and are only a few in the periphery. Cones are densely packed in the Fovea of the retina. The red, green and blue colors are detected by three different cone cells. The blue color generates maximum brightness of 2.56 to 2.76 eV and the red color is the least, generating 1.65 to 1.90 eV. These three cone cells make a unit known as the Trichrome unit. By various combinations of the impulse generation by the trichrome units, we are able to perceive the entire color spectrum. This is the basis of the printers' color cartridges we are so familiar with. The pigment of the cone is called Opsin. It is a protein and it is most sensitive to light waves with a wavelength of 550 nm, blue responds to light waves with a wavelength of 450 to 485 nm and green to 500 to 565 nm wavelength.
White and Black color.
There is no black color receptor. Instead, black, white and gray color perception depends on various shades of gray colors. The pigment of the gray scale is Rhodopsin, and the receptors are known as Rods. Rods are most plentiful at the periphery of the retina and are only sparsely distributed in the central part of the retina. Rhodopsin is most sensitive at light waves of 555 nm.
We see better in the corner of the eyes when light is very faint. There are no cones at the periphery of the retina, which is the reason we are unable to see color in the dark.
Why are black and white images not as clear as a color picture.
Each cone is connected with one neuron of the retina that sends out stimuli to the brain. 5 or 6 Rods are connected with one nerve cell, as a result, color picture has more pixels so to speak, and is sharper and clearer than black and white images.
Upside down and revered sidewise image.
This diagram illustrates why the upside down and left side on the right side image projected on the retina.
This is a pinhole camera taking a picture of a tree. The same Laws of Optics work for the eyes.
How the Brain rights up images.
A newborn child grabs things with hand and tries to put them in his /her mouth. That is the beginning of the learning process of the brain and by the time the baby is 2yr old the proper interpretation of images by the brain is nearly complete but the learning process of the brain continues for lifelong.
Near and Distant vision.
Refractive errors of one or more components of the eye (cornea, anterior chamber, lens and vitreous) fail to bring light precisely on the retinal receptors and when the light rays fall short- then the condition is known as Near- Sightedness and when the light rays converge beyond the light receptors then it is called Far- Sightedness.
Double vision.
Double vision may be monocular or binocular. Mono-ocular double vision comes from the eyes, or contact lens injury, or foreign body injury of the cornea.
Binocular double vision is due to the failure of mages to merge into one. The defect may lie anywhere from the optic nerve to the visual cortex. Since eyes are extensions of the brain and when an eye is damaged it may not improve unless treatment starts immediately.
A quick way to determine mono-ocular or binocular double vision
The mono-ocular double vision disappears when the eye producing the double vision is closed and the person looks through the other eye. In binocular double vision persists by closing and opening one eye at a time.
In daylight, our world appears in full complements of spectrum colors - clear and beautiful and images up-righted and sides correctly positioned. In the dark the story is different. In fading light, the world appears in various shades of gray, fuzzy and best visible to us by the corner of the eye provided one is neither near-sighted nor far-sighted.
*******************************************************
***