Cytomegalovirus;
P.K. Ghatak, MD.
Cytomegalovirus.
Cytomegalovirus belongs to the Beta Herpesvirus group. Cytomegalovirus is species specific. Herpesvirus 5 is a Human Herpesvirus. Genome specific virulence is characteristic of this virus. It prefers to grow in human fibrocytes and produces a large inclusion body. This gave this virus its name as " large cell” Cytomegalovirus 5 (CMV). Once inside the human body, it produces primary infection and after the infection subsides, CMV hibernates in lymphocytes, monocytes, dendritic cells and CD34+ cells and remains dormant for the entire life of the person.
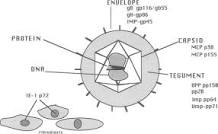
The virus is large, has a diameter of 200 nanometers and the nucleus contains double stranded DNA and the virus is shaped like a disk. CMV has a large genome with an icosahedral capsid and a dense core surrounded by an amorphous matrix.
Humans are infected in several ways –
1. During close contacts with an infected person.
2. From saliva and ingestion of contaminated food and drinks.
3. Via blood transfusion, bone marrow and solid organ transplantation.
4. Sexual contact.
5. Placental transmission to fetus.
6. Through breast milk.
The percentage of the population infected with CMV varies from 100% in underdeveloped countries to 40 to 60 % in advanced nations.
The incubation is 8 days to 8 weeks, the majority of infections, in both healthy children and adults, produce minor cold symptoms or no symptoms at all. The only evidence of infection is the séropositive.
In Immunodeficient patients:
The infection is widespread in immunodeficient patients and people on immunosuppressed drugs. CMV infects any organ of the body and in the majority of cases, most organs are infected and the outcome is generally bad. Cell mediated immunity is the primary defense against CMV infection. HIV infection and other clinical conditions where CD4+ and CD8+ cell counts are low, the widespread infection is common. Even after a successful antiviral therapy, the recurrence of infection and chronic infection are common.
CMV remains dormant within the cells and reemerges following other viral infection or other illnesses. This characteristic is similar to varicella virus, Epstein Barr virus and Toxoplasma gondii (a protozoa).
Clinical picture:
The young symptomatic patients present with fever, pharyngitis, cervical adenopathy, and upper and lower respiratory infection. A morbilliform skin rash is generally present, however, skin rashes of various other kinds are also seen. Blood tests may show atypical lymphocytes but the heterophile antibody test is negative (modified Paul Bunuel Test)
In more serious infections, hemolytic anemia and thrombocytopenia are present. Gastritis and colitis may develop. When GI and urinary systems are infected, a prolonged viral shedding is a common occurrence. Meningoencephalitis, myelitis, retinitis, uveitis, and neuropathy are some of the serious aspects of nervous system infection.
The CMV infection is difficult to differentiate on clinical grounds from Infections Mononucleosis. In CMV, the fever generally lasts longer and lymph node enlargements are less extensive.
The definitive diagnosis is by detecting DNA of CMV by the PCR method. Blood, urine, and saliva are suitable for PCR tests but a blood test gives the most conclusive evidence of CMV infection. In post-transplant patients, tissue biopsy is the preferred test.
Important clinical situation of CMV infection.
A. Congenital CMV (cCMV) infection.
B. Stem cell transplantation in hematological malignancy and solid organ transplantation.
Congenital CMV infection (cCMV).
If a previously uninfected pregnant woman acquires CMV infection in the first trimester, the virus infects the placenta and then infects the developing embryo. Two areas of infections are most critical.
1. Brain development abnormalities and related symptoms
2. Sensory deafness and blindness.
Congenital CMV brain and clinical features (cCMV)
Microcephaly, seizure disorder, cerebral atrophy, cystic lesions in the temporal lobes, periventricular calcification and dilated cerebral ventricles, and demyelination. Delayed fetal growth is common.
These changes clinically resemble Cerebral palsy, Multiple sclerosis, Peripheral neuropathies, Leukoencephalomyelitis, and Aicardi-Goutières syndrome (a rare congenital gene mutations resulting in deformed brain and skin lesions).
2. The cCMV is the leading viral, non-genetic, cause of congenital sensory deafness.
Congenital eye infection is a leading cause of childhood vision problems and blindness. Chorioretinitis, uveitis, ophthalmitis and optic atrophy are manifestations of CVM infection. Blindness is due to optic atrophy and detached retina from fibrosis as chorioretinitis heals.
B. Stem Cell Transplants and Solid Organ Transplants, and their relation to CMV.
General consideration.
The CMV status of the recipients is determined by the presence of IgM and IgG antibodies. In allogeneic hemopoietic stem cell transplants, the donor CMV antibody status and immunohistopathology examination of tissue are collected. After the transplantation, if recurrence of CMV is suspected, several additional tests are performed. Presence of Leukocyte CMV pp65 antigen indicates infection and QNAT (quantitative nucleic acid test) is done to determine the viral load.
In both stem cell and solid organ transplants, if the recipient is seropositive, but the donor is seronegative, then the outcome of the transplant is the best. The worst outcome in a situation where the recipient is seronegative and the donor is seropositive. CMV virus reactivates because the use of immunosuppressive drugs depresses T-cell count. Immunosuppression is needed to prevent transplant rejection. The graft versus host disease is another cause of reactivation of CMV. Loss of life occurs in overwhelming CMV infection.
T-cell and Hemopoietic transplant.
During the pre-transplant phase, a high dose of immunosuppressive drugs is used to wipe out all malignant cells from the body. The T-cell count falls to the lowest levels. This is the prime reason for the subsequent reinfection.
Prophylaxis against CMV infection.
The choice of drug is Valganciclovir. It is an oral prodrug of Ganciclovir. Ganciclovir is converted to triphosphate form and inhibits DNA replication of CMV. It can produce cytopenia.
Acyclovir is also used. It is given 800 mg 4 times a day for 12 weeks. Nephrotoxicity and cytopenia are the main side effects.
Other drugs:
a. Letrovir. It inhibits viral terminase enzyme and thereby viral replication. Leterovir can be used more than 100 days without any additional side effects.
b. Foscarnet. It is a phosphate analog of ganciclovir. It inhibits the polymerase enzyme. Furthermore, it is less toxic to bone marrow.
c. Mribavir. It is a benzimidazole antiviral drug. It prevents viral UL97 enzyme. It inhibits viral polymerase.
d. Cidofovir. It is anucleotide analong inhibits polymerase enzyme, given IV weekly.
e. Brincidofovir. It is an oral analog of Cidofovir.
Adoptive T-cell therapy.
Harvested T cells, matched for HLA, are incubated with specific CMV antigen protein. The engineered T-cells are made to multiply in large numbers and then transfused. This is a newer method to control infection in CMV resistant to all drugs.
Vaccine:
A vaccine – Transvax contains a viral plasmid that encodes pp65 and gB glycoprotein, is in use in a pilot study. Two other vaccines, CyMectin and AVX601, contain a viral DNA subunit and use a vector to deliver it.
Treatment of CMV infection/recurrence.
Drug of choice for treatment of CMV viral infection and recurrence is Ganciclovir. Ganciclovir is given 5 mg/Kg/ every 12 hrs. for 14 to 21 days.
Acyclovir is effective but the response in individual patients varies. It is given IV 500 mg per square meter of body surface every 8 hrs. for 2 weeks. A small amount of TNF given with Acyclovir greatly increases the therapeutic effects of acyclovir.
****************************************************

No comments:
Post a Comment