Creatine / Creatinine and Kidney
PKGhatak, MD
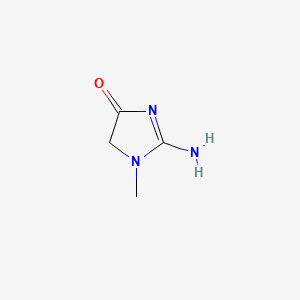
Creatine is an amino acid, chemically it is methylguanidoacetic acid. Creatine is mostly present in skeletal and heart muscles and in small quantities in the brain and testes.
Creatinine is the metabolic end product of creatine. Creatinine is formed in the muscles from anhydrous creatine by a non-enzymatic removal of H20 and intramolecular cyclization.
Blood levels of Creatinine - for men 0.75 to 1.5 mg/dL or 65 to 119 micromoles/L/L and for adult women -0.6 to 1.04 mg/dL or 52 to 92 micromoles/L.
The creation comes from two sources. A. Biosynthesis. B. Form diet.
A. Biosynthesis:
It takes place in two stages and in two places. The kidneys are the main place of biosynthesis in the first stage. However, when both kidneys are removed, about 15 % of the biosynthesis of creatine takes place in the pancreas.
The enzyme L-Arginine-Glycine-amidinotransferase catalyzes Glycine + Arginine to form Guadinoacetetic acid and Ornithine. Guadinoacetic acid, known as Glycocyamine and is transported by a carrier protein to the liver.
Control of biosynthesis.
GI source of creatine has a negative feedback effect on the renal enzyme guanidinoacetate. When GI absorption is high, renal production of guanidinoacetate is reduced proportionally but this has no effect on the production of creatine in the liver. However, creatine synthesis in the liver is dependent on kidney transamidase activity and hepatic synthesis is reduced as less glycocyamine is available in the liver.
Hormone influence.
Hyperthyroidism slows kidney transamidase activity due to high blood creatine levels.
Genetic mutation:
Mutation of the gene causing transamidase deficiency, an inborn error of creatine synthesis, is characterized by language, cognitive and behavior disorders.
B. In the liver Guadinoacetetic acid reacts with S-adenosylmethionine by enzyme methyltransferase and from Creatine and Adenosylhomocysteine. Methionine is the principal methyl donor; other minor methyl donors are choline and betaine. This reaction is not reversible. Glutathione and other reducing substances are required for the optimal activity of this enzyme.
B. Dietary source of creatine.
Food rich in guadiniacetic acid (GAA) is meat, poultry, fish, milk and milk products, and apple and loquat. Of the total turnover of 2 gm per day, a normal diet supplies only 5 % of GAA. The rest comes from biosynthesis.
Creatine in the muscles:
Creatine is transported to muscles and upon entering the muscle cells, creatine is acted upon by ATP ( adenosine triphosphate) to turn it into Creatine phosphate by ATP-creatine-phosphorylase enzyme. Creatine phosphate becomes cell bound and can not escape the cell. It is a high energy molecule, that easily transfers high energy phosphate to ADP when the muscle is contracting rapidly and exhausts all ATP. Conversion of ADP to ATP is catalyzed by adenyl kinase. Lactate and acetate block this reaction when these organic acids accumulate in muscles during prolonged activities. In the heart, the myocardium is capable of sustaining activities by utilizing fatty acids. lactate and ketone as fuels.
In the resting stage, muscle contains 6 times as much creatine-phosphate as ATP. Creatine phosphate is proportional to the body's muscle mass. In the muscles, 85 % of creatine is present as creatine phosphate. And all the creatine produced by the muscles is excreted in the urine. And the 24-hour urinary creatinine is remarkably constant in an individual.
Interest in improving muscular performance by creatine.
Sports :
Athletic performance is enhanced by a higher concentration of creatine-phosphate in the muscles and creatine is used as a nutritional supplement to that effect. Creatine supplement is available as creatine citrate, creatine monohydrate and creatine pyruvate.
Experimental use of creatine in diseases:
In ALS, Muscular dystrophy, and Multiple sclerosis, creatine supplements are used but no significant improvement is noticeable.
Creatine ethyl ester(CEE):
A new form of creatine supplement, creatine ethyl ester, is available. It has an advantage over other forms because it resists degradation in the stomach and bioavailability is greater. It is soluble in fat and has much higher membrane permeability. It is slowly metabolized and so muscle performance can have a quicker onset and be more sustained at a high level of performance.
The half-life of creatine is 3 hrs. 3 to 6 hourly dosing is necessary in order to maintain high muscle creatine concentration. Once the supplement is stopped, the muscle creatine returns to baseline in 4 weeks.
Renal Excretion of Creatinine.
Creatinine in the blood is derived as the end product of creatine phosphate metabolism in the muscles. Creatinine is water soluble and readily filtered by the glomeruli of the kidney; about 15 % of creatinine is secreted by the cells of the proximal renal tubules in healthy adults. In renal failure, the tubular secretion may increase to 30 %, and some creatinine loss takes place through the intestine.
Effect of high protein diet.
A normal diet contains creatinine of about 1/10th of the daily requirement of creatine. When placed on a high protein diet, the fecal loss of creatinine rises sharply and creatinine only minimally.
Serum creatinine and creatinine clearance capacity of the kidney:
The Glomerular Filtration Rate (GFR) of Creatinine is considered the standard test of renal filtration capacity in health and in diseases. Any reduction in GFR is an indication of renal disease.
To detect the true glomerular filtration capacity, the test material must only be filtered by the kidney and should not be secreted either by renal tubules or the intestine. Creatinine is not ideal from that point because it is also lost in other ways as stated above.
Such an agent was Inulin. Inulin is a complex carbohydrate, obtained from the roots of the Chicory plant. In earlier times, Inulin clearance was the gold standard for renal filtration. It is now abandoned because of multiple factors including the very high cost of conducting tests requiring a hospital stay.
Then several radioactive agents were introduced. These tests were also given up due to concerns about radiation exposure to patients and clinic personnel.
Creatinine Clearance Test (CCT) is now accepted as GFR in health and in renal diseases.
Modified creatinine clearance test.
A standard CCT requires the meticulous collection of 24 hrs.' urine and several blood creatinine level determinations.
Soon a simpler test came into medical practice, which is equal to the standard CCT in every respect if not better. The modified CTT is done by deduction. The GFR is determined from one serum creatinine level.
The formula of GFR is -
For adult males:
GFR = 141 x (Scr/79.6) – 0.41 x (0.993)Age.
For adult females:
GFR = 144 x (Scr/61.9) – 1.209 x ( 0.993)Age.
Scr = serum creatinine in micromoles per liter.
[ Conversion table- mg/dL to micromoles/L of creatinine.
1mg /dL of creatinine = 0.01131222 micromoles /L.]
Correction factors are available for non-white races.
Normal GFR is above 60 ml/min and usually 80 to 160 ml/min
Other formulas:
CKG -EPI Creatinine Equation 2021.
eGFR =
142* min(standardized Scr/K, 1)α * max(standardized Scr/K, 1)-1.200 * 0.9938Age * 1.012 [if female]
eGFR (estimated glomerular filtration rate) = mL/min/ 1.73 m2 ( m 2 = square meter)
Scr (serum creatinine) = mg/dL
K = 0.7 (females) or 0.9 (males)
α = -0.241 (females) or -0.302 (males)
min = indicates the minimum of Scr/K or 1
max = indicates the maximum of Scr/K or 1.
Calculate serum creatinine from GFR
eGFR= mL/min/1.73m 2 ( m 2 = square meter)
Serum Creatinine * µmol/L.
The typical range for serum creatinine is: For adult men, 0.74 to 1.35 mg/dL (65.4 to 119.3 micromoles/L) For adult women, 0.59 to 1.04 mg/dL (52.2 to 91.9 micromoles/L).
Latest method.
An iodinated compound, Iohexol, is a safe contrast agent used in radiological studies. Iohexol is now used for GFR determination. Iohexol does not combine with blood proteins and is well distributed in the body. It is excreted by glomerular filtration only. No other renal or GI process is involved in the excretion of Iohexol.
After giving a loading dose by IV at the clinic, the subject/patient is sent home to collect blood samples on supplied papers from fingertip puncture,( very much like the Glucose home test) at certain intervals. And when the test is completed, dried blood samples on paper are mailed back in a prepaid envelope. The Iohexol concentration in the dried blood samples is determined by Liquid Chromatography. And the GFR is calculated by a given formula. Recently, the American Diabetes Association recommended the Iohexol GFR test on an annual basis in diabetics. This test is called Dried Blood Spot (DBS) for GFR.
Stress Tests for Kidneys.
Like cardiac stress tests, Kidney Stress Tests are possible. Kidney stress tests are generally not done in clinical practice but are important for drug manufacturers and researchers.
These are some of the kidney stress tests.
High protein diet test. To test the GFR. 2. Creatinine load test. To test the proximal tubular cation transfer ability. 3. Water restriction test. To test the kidney's ability to concentrate urine in the collecting tubules. 4. Ammonium chloride loading test. To study H ion retention ability. 5. Oral bicarbonate load test. To study H ion handling capacity.
If one is due for a blood test, which includes serum creatinine, on making a request for a copy of test results at the time of registration, the lab will test the results. On a closer look, one will find an estimated GFR at the bottom. If GFR is a bit low, no need to be disheartened. The lab might have given the results based on a formula that takes the Body Surface Area into account. And sure enough, the lab did not take height and weight. So recalculating the result with actual height and weight might give a better GFR number.
*****************************************************************


No comments:
Post a Comment