Peptic ulcer disease.
PKGhatak, MD
When ulcers develop in areas of the stomach normally bathed by acid and pepsin, those ulcers are called peptic ulcers. All sections of the stomach and the first part of the duodenum come in contact with acid and pepsin. And occasionally in an incompetent lower esophageal sphincter, the lower end of the esophagus develops ulcers due to gastric reflux.
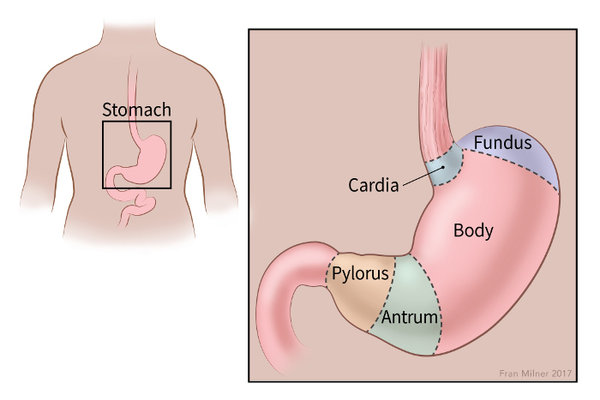
Typically, peptic ulcers are found in the first part of the duodenum and the Pylorus.
It is estimated that about 4 million new cases are detected annually worldwide. In the USA, about 5 to 8 % of the population have peptic ulcer disease. In the past several decades, the incidence of peptic ulcer fell but in recent times, the incidence has remained steady.
Gastritis and gastric erosion are included in Gastric ulcer diseases because the mechanism of development of these is the same as ulcers.
Why do people develop Ulcers of the stomach.
The immediate cause of peptic ulcer is excess acid and protein digestive enzyme pepsin production by the cells of the mucous membrane of the stomach.
Risk factors of peptic ulcer disease.
1. Infection of Helicobacter pylori (H. pylori).
2. Cigarette smoking.
3. Alcohol abuse.
4. Chronic use of aspirin or non-steroidal anti-inflammatory drugs (NSAID).
5. Anxiety and stress.
6. Use of systemic steroids.
Peptic ulcer.
The common practice today is to detect peptic ulcers by endoscopy. Any area of the stomach and duodenum that appears abnormal under endoscope is usually biopsied and the histology of the tissue is examined. Gastritis and ulcers due to H. pylori can be detected and if any doubt exists, a biopsy should be enough to exclude cancer.
Peptic ulcers are small, less than 1 cm in diameter, have clear margins and a clean base. Cancers are usually located in the cardia and fundus of the stomach, usually large, and the margins are heaped up, the base is necrotic.
Panel A: are benign lesions. Panel B: is a cancer of the stomach.
A brief review of the characteristics of the gastric mucosa.
The inner lining of the stomach is called the mucous membrane. The diagram below shows the relative thickness of the stomach wall and a cutout section shows the different cells in the mucous membrane.

The function of the cells of the mucous membrane.
1. Parietal cells. These cells produce a strong inorganic acid - hydrochloric acid. The pH of the stomach is 1 to 2. Parietal cells also produce the Hematinic principle, a glycoprotein, which is essential for Vitamin B12 absorption.
2. Chief cells. Chief cells secrete an inactive form of protein digestive enzyme, Pepsinogen. Pepsinogen at pH 1 or 2 is converted to an active enzyme, Pepsin. And pepsin remains active in pH 1 to 8.
location of endocrine cells, stained brown.
3. Endocrine cells. The endocrine cells are G-cells, ECL-cells, and D-cells.
G-cells secrete Gastrin directly into the bloodstream. (that is the nature of all endocrine glands and cells). Gastrin is brought back to the mucosa by circulation. Gastrin stimulates the growth and development of parietal cells and enterochromaffin-like cells (ECL) cells.
ECL-cells produce and store Histamine and secrete histamine. Histamine is a potent stimulant for acid secretion. In addition, ECL cells secrete chromograninA derived peptides, pancreastatin and other peptides.
D-cells. D-cells secrete Somatostatin. It is an inhibitory hormone. It decreases the release of gastrin and decreases the motility of the stomach and intestine. Also delays the release of other peptides from ECL cells.
5. Goblet cells and mucus secreting glands. Goblet cells secrete mucus. The mucus has a very significant function. The mucus is of two layers, one of which is adherent to the cell layer and the free layer on the top of the adherent mucus layer. Both layers are about 1 mm thick and chemically are glycosylated mucin peptides. It contains a high concentration of bicarbonate ion [HCO3-]. HCO3 is immediately available to neutralize any HCl (hydrochloric acid) that comes in contact with the mucus layer.
The mucus barrier acts as a cushion on which gastric juice floats. It is like an atom or a proton kept separated from the copper tube and confined to a narrow zone by powerful electromagnets in a cyclotron (atom smashers).
Acid production in the stomach.
The parietal cell contains the Carbonic Anhydrase enzyme. This enzyme greatly accelerates the reaction between H20 +CO2 -->H2CO3, taking place within the cell cytoplasm. H2CO3 then dissociates into H ion [H+] and HCO3 ion [HCO3-]. Energy dependent [Na+]/[H+] pump (commonly called Proton pump) expels [ H+] into the stomach lumen and in exchange [K+] enters the cells. [HCO3-] is carried from the cells into the blood by a cation exchanger transport protein and it brings back [Cl-] inside the cells. [Cl-] enters the gastric lumen via Cl channels. [H+] unites with [HCO3-] because opposing charges attract each other and form HCl.
Factors accelerate Acid production.
The Vagus nerve is the secretory motor nerve for the GI tract. As soon as food enters the stomach, vagal stimulation produces Acetylcholine. Acetylcholine directly stimulates gastric acid secretion and indirectly by increasing gastrin release.
G-cell.
Stimulate acid production via gastrin.
Histamine.
Histamine is a potent stimulant for vasodilatation, increased glandular secretion, and other properties. In the stomach, the Histamine is produced and released by ECL- cells, nerve cells and mast cells. Histamine 2 receptors are present on the surface of the Parietal cells. Once histamine combines with the H2 receptors, acid production increases. Histamine is the main regulator of acid secretion influenced by local conditions.
D- cell.
D-cell produces Somatostatin. It inhibits acid production and decreases gastric motility and other inhibitors control beyond the stomach.
Conditions favor peptic ulcer.
Smoking.
Cigarette smoke contains Nicotine. Nicotine decreases Prostaglandin generation and makes gastric mucosa vulnerable to ulcer formation.
Alcohol.
Alcohol is a poison to cells when it comes in direct contact with cells. Alcohol destroys the mucus coat of the stomach, making it easier for alcohol to come in contact with the mucosa. An excessive amount of alcohol produces gastritis and chronic use produces ulcers. Once peptic ulcers are formed, even a small amount of alcohol damages cells and prevents ulcer healing and causes pain.
Aspirin.
Aspirin on ingestion turns into salicylate. Salicylate is toxic to cells and produces erosion of surface cells, disrupts the H+/K+ pump and loss of K+ from the cells. Hemorrhagic gastritis and gastric ulcers are common adverse effects of aspirin.
Since aspirin inhibits the enzyme cyclooxygenase permanently for the life of affected cells, adverse effects persist even after aspirin is withdrawn.
NSAID.
Non-steroidal anti-inflammatory drugs are commonly prescribed (e.g. Advil) for joint and bone injuries, post orthopedic surgery, and all varieties of arthritis and are also available as OTC (over the counter drugs). Peptic ulceration and gastritis have increased in recent years, going against the trend seen in several past decades.
NSAID inhibits the COX-1 enzyme. COX-1 is another enzyme needed for Prostaglandin synthesis. The effect of NSAID is however temporary, once the drug is stopped, the cells can recover.
Helicobacter pylori (H.pylori).
H.pylori is a gram negative, highly motile, unipolar-multi flagellated, microaerophilic organism. The body of H. pylori is spiral and so it is called Helicobacter. Scientists believe H. pylori infected the stomach of humans 2,5000 years ago and is still infecting humans. More than 50 % of the world's population is already infected, and 100 % of people in Africa and Asia have H. pylori chronic gastritis, although 80% are asymptomatic. Most people are infected in early childhood by the oral-oral route and the fecal-oral route. Once infected, 80 % of the bacteria are present in the mucus of the gastric lumen and 20% in the mucus secreting cells of gastric epithelium but absent in the parietal cells, endocrine cells and the chief cells of the epithelium.
The bacterium has developed a unique mechanism of evading the immune defense of the victims and continually inventing ways to resist antibiotics. The bacterial wall has several layers of envelopes of different proteins and in addition, has several adhesion proteins and these proteins keep the bacteria firmly attached to the cells.
Detection.
Breath test.
The human body does not have urea splitting enzyme urease, but H. pylori contains urease that breaks down Urea into CO2 and ammonia. A tablet containing 13C urea and citric acid is taken by mouth and the expired air is collected and analyzed. Presence of C13- CO2 in expired breath indicates H. pylori infection.
Biopsy.
Patients present with symptoms of peptic ulcer usually undergo endoscopic examinations. Biopsy from the suspected areas is taken. H.pylori is easily detected, if present.
Treatment.
Because antibiotic resistance is common, the antibiotic regimen is often changed. A commonly used regimen is mentioned and also a reference to the 2022 recommendation is provided.
Antibiotics:
Amoxicillin and one of the following two antibiotics: Macrolides and Metronidazole (an anaerobic bacterial antibiotic). Antibiotics are combined with Bismuth subnitrate. Bismuth forms a complex with the bacterial wall, inhibits multiple bacterial enzymes resulting in decreased synthesis of adherence protein molecules and deprives H. pylori source of nutrition.
Acid suppression.
Pantoprazole. It blocks the proton pump and acid secretion comes to a total stop.
Histamine receptor blockers. It acts by competitive binding with H2 receptors of the parietal cells and blocks the action of histamine in producing acid.
Antacids. Commonly used aluminum oxide and calcium carbonate as acid neutralizers are not therapeutically sufficient in the treatment of peptic ulcers.
____________________________________________________
https://www.gastroenterologyandhepatology.net/archives/june-2022/helicobacter-pylori-treatment-regimens-a-us-perspective/
(Copy & paste on your browser.)
*******************************************




No comments:
Post a Comment