Blood
flukes
P.K. Ghatak, M.D
Blood
Fluke infection is the 3rd
flatworm (Trematode) parasitic disease of humans discussed
here, Liver fluke and Lung fluke were the other two mentioned in
the earlier blogs.
Schistosoma
hematobium is the parasite and the disease produced by the worm is
called Schistosomiasis, also known as Bilharziasis and Snail fever.
Schistosoma means a split - body. The shorter and stouter adult male
has a longitudinal cleft along the length of the body and in that
space, a slender, longer female worm is held in embrace by the male
for its life. A German doctor, Theodor Maximilian Bilharzia, while
serving in Egypt, discovered the flatworm parasite in 1851, and the
disease is named after him.
Two
distinct illnesses are produced by Schistosoma species.
Urogenital Schistosomiasis. Produced by S. hematobium. The worms reside in the venules (small veins) of the urogenital organs.
Gastrointestinal & Biliary Schistosomiasis. Several Schistosoma species are responsible and they are named according to the initial case originating country. The parasites invade the venules of the GI and biliary systems.
The
life cycles of all the species of Schistosoma are identical and
closely resemble those of the other trematodes.
Humans
are the final host and act as the reservoir of the parasite. Other
primates, ruminant farm animals and rodents are additional reservoirs.
Incidence
of Bilharziasis.
The
WHO estimates 200 million active cases are seen annually.
Genitourinary bilharziasis is common in the Nile River Valley of
Egypt and the adjoining northern African countries. Gastrointestinal/biliary bilharziasis occurs in China and countries surrounding the
South China Sea. It is also prevalent in South America and the Caribbean
islands. Indigenous bilharziasis does not happen in the USA.
Life
Cycle of Schistosoma.
Human
and animal feces and urine contaminate rivers, lakes and other bodies
of water. Digging canals for irrigation has spread the risk of
bilharziasis in much wider areas. Inundation during the rainy season
is another hazard.
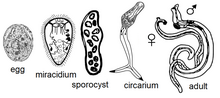
Schistosoma
development stages are - Egg, Miracidia, Sporocyst, Cercaria and Adult.
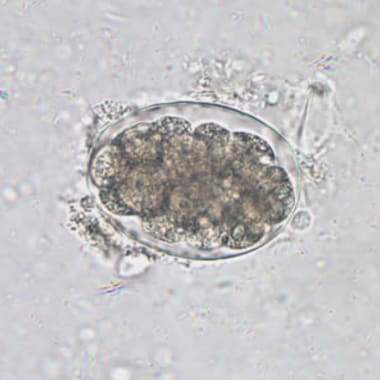
Eggs:
An embryonated egg has a spine, and the position of the spine distinguishes
one species from the other. Each egg is elongated or oval, measuring
about 175 X 45 micrometers. Inside an egg, one embryo is in the
development stage. A hinged door at the head-end opens and lets a
grown larva out in the water.
Embryos:
Miracidia larva is 200 micrometers long and covered with cilia and is
a free swimmer. Miracidia larva lives in the water only a few hours
and must find the proper snails that live in sweet water to multiply and develop further into infective larvae.
Sporocytes:
Miracidia after entering inside the snail, move to softer tissue
and transform into cysts. Cyst develops many daughter cysts and
the daughter cysts move to newer locations and continue to develop
into Cercaria larvae.
Cercaria
larva is 500 micrometers long, has a tapering head and a forked tail.
Cercariae live only 3 days. It takes only a few minutes for cercariae to enter into the body of their victims by penetrating the skin. It
drops its tail and moves inside the veins. Inside the blood vessels,
it becomes a round ball and is carried by the blood to the heart, lungs, and
finally to the liver. In the liver, cercariae develop in about 3 weeks
into adult male and female worms.
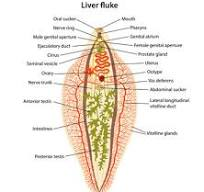
Adult
worms: Adult worms are 7 to 29 mm long, have a cylindrical body,
colored gray-white, have two suckers and an alimentary canal but no
anus and the body is filled with reproductive organs.
Subsequently,
the life of Schistosoma depends on the species and victims.
|
Schistosoma species
|
Definitive host
|
Site of infection
|
Eggs discharged in
|
Endemic area
|
|
S. hematobium
|
Humans, other primates
|
Genitourinary system
|
Urine
|
Africa
|
|
S. japonicum
|
Humans, carnivores, ruminants | GI & biliary mesenteric veins
|
feces
|
South-East Asia |
S. mansoni
|
Humans, rodents
|
As above
|
feces
|
Africa
|
|
S.mekongi
|
Humans, dogs
|
As above
|
feces
|
South-East Asia
|
|
S. intercalatum
|
Humans, rodents and cattle | As above
|
feces
|
South-East Asia
|
Symptoms:
The initial infection produces no symptoms. Some people develop an itch at the skin penetration sites and it is called swimmers' itch. Some
others develop eosinophilia and patchy pneumonia.
Acute
symptoms. Eggs produce allergic reactions known as Katayama fever. It
manifests as fever, weakness, fatigue, and lymphadenitis.
Abdominal
pain, low grade fever and eosinophilia develop in others.
Chronic
symptoms. Many eggs are carried away to different organs. The eggs
get embedded in the tissues and generate immune reactions. The initial inflammatory reaction is followed by tissue necrosis, fibrosis
and granuloma formation. Small granulomas coalesce together into
polyps. Polyps are seen in the urinary bladder and esophagus, stomach and intestine.
Genitourinary Bilharziasis: Hematurrhea, painful urination, urinary tract
infection, glomerulonephritis, deformed external genitalia, calcified
lesions surrounding the embedded eggs in tissues, specially in the
urinary bladder, are common. Carcinoma of the bladder also develops.
Fibrosis of the various components of the reproductive organs leads
to difficulty in pregnancy and miscarriage. Blood in semen in a male patient is a
striking feature.
Gastrointestinal and biliary bilharziasis:
Abdominal
pain and diarrhea, dysphagia, bleeding varies in the esophagus and
stomach producing anemia and malnutrition. Liver and spleen enlargement, anemia and leukocytopenia develop due to hypersplenism.
Calcifications of blood vessels lead to various ischemic symptoms.
Distal
organ involvement:
CNS.
In the brain, the eggs are calcified and cause seizures, headaches and
paralysis of limbs.
In the
spinal cord: Transverse myelitis is a serious problem
Lungs:
In the chronic stage, Pulmonary artery stenosis and calcifications produce
pulmonary hypertension.
Heart:
Myocarditis and heart failure occur.
Diagnosis:
Stool examination detects eggs and the shape of eggs and the
characteristics of the spine help diagnose the Schistosoma species.
Egg
characteristics:
S.hematobium
– Eggs are oval-shaped, the spine is long and sharp and attached to
the terminal end.
S.
japonicum - Eggs are round. The spine is rudimentary and
appears like a hook and is attached to the lateral side.
S.
mansoni –Eggs are elongated and the spine is attached at the
posterior end of a side.
S.
mecongi – Eggs are 30–45 micrometers long and have a short lateral
spine.
S.
intercalatum – Eggs are oval-shaped and the spine is attached to the
terminal end; Its eggs resemble S. hematobium eggs.
In S.
intercalatum infection, few eggs are excreted in the feces. The
infection is in the lower colon and rectum. A biopsy of the rectum is
required.
In CNS
infection, more reliable tests are ELISA antibody test and parasite DNA
identification by PCR test.
Treatment:
Praziquantel is a very effective drug in killing adult worms but immature worms are not killed. A person is usually infected
repeatedly, and both mature and immature adult worms are present at
the same time. So Praziquantel is repeated weeks later. The Cure
rate is 90 %.
Special
features of Schistosoma. The adult worm does not produce inflammation
or allergic reactions, only the eggs are allergenic.
The
adult worm is classified as a flatworm, but it resembles round worms. The worms, unlike other flukes, are not hermaphrodites, the male
and female sexes are separate.
****************************
.
in
other primates, ruminants, rodents and cattle.
Adult
The
adult worms are 1–2 cm long with a cylindrical body that features
two terminal suckers, a complex tegument, a blind digestive tract,
and reproductive organs
Schistosoma spp. [these
species cause schistosomiasis/bilharzia in humans and ruminants]
Parasite
morphology: Blood
flukes form five different developmental stages: eggs, miracidia,
sporocysts, cercariae and adult worms. Eggs are round to oval in
shape, operculate (hinged at one end) and contain a developing
embryonic larva (miracidium). Differences in egg morphology can be
used to distinguish between Schistosoma species: S.
mansoni producing
oval eggs (115-175 x 45-7µm) with a sharp lateral spine, S.
japonicum forming
round eggs (70-100 x 50-70µm) with a rudimentary lateral spine;
and S.
haematobium producing
oval eggs (110-170 x 40-70µm) with a sharp terminal spine. Miracidia
are elliptical free-swimming larval stages (~200µm long) covered
with cilia. Sporocysts appear as pleomorphic sac-like bodies which
contain developing cercariae. Mature cercariae are elongate
free-swimming larval stages (400-600µm long) consisting of a
tapering head (with prominent penetration glands) and a forked tail
(furcocercous). Adult flukes are elongate tubular worms (10-20mm
long), with rudimentary oral and ventral suckers. Males are shorter
and stouter than females, and they have a longitudinal cleft
(gynecophoral canal or schist) in which the longer slender female
lies folded.
Theodor
Maximilian Bilharz
Regarding
Katayama syndrome (a possible clinical manifestation of
schistosomiasis in naive patients characterized by fever, cough,
myalgia, headache and abdominal tenderness [19]),
descriptions fitting its clinical manifestations can be found in
ancient books of traditional Chinese medicine referring to more than
2400 years ago